
Benzodiazepine Dependency
Heather Ashton, DM, FRCP
1997

School of Neurosciences
Division of Psychiatry
The Royal Victoria Infirmary
Queen Victoria Road
Newcastle upon Tyne NE1 4LP
Eds. A Baum, S. Newman, J. Weinman, R. West, C. McManus,
Cambridge University Press, 1997, pp. 376-80
The Ashton Manual · Professor Ashton's Main Page
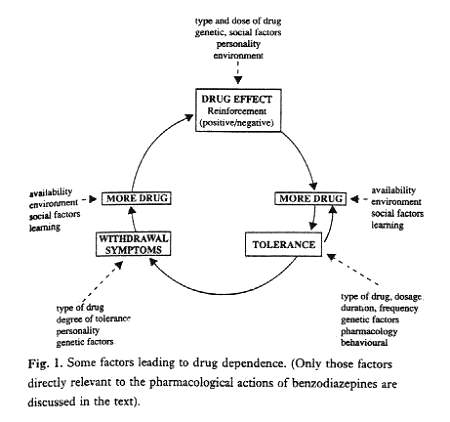
Drug dependence has always been difficult to define. This complex condition, which may develop after repeated use of some psychoactive drugs, involves variable combinations of at least three interacting factors: (i) an emotional state consisting of a craving or compulsion to continue taking the drug, either for its directly rewarding (reinforcing) properties or to avoid the discomfort of its absence, (ii) a behaviour consisting of compulsive drug-taking or drug-seeking, and (iii) a physical state which may include drug tolerance and an abstinence syndrome with somatic and/or psychological symptoms. A drug-dependent individual eventually becomes enmeshed in a self-replicating loop upon which many other factors impinge (Fig. 1).
TYPES OF BENZODIAZEPINE DEPENDENCE
In the case of benzodiazepines the definition becomes doubly difficult for there are at least two types of benzodiazepine dependence: (i) low dose dependence on medically prescribed benzodiazepines and (ii) high dose dependence on illicitly obtained benzodiazepines. In low dose dependence, patients receive long-term prescriptions from their doctors in clinically recommended oral doses, often over periods of 20 years or more. There is a slight tendency to escalate dosage over the years but prescriptions usually remain within therapeutically recommended limits. The drugs are used initially for their anxiolytic or hypnotic properties and later to prevent perceived or anticipated withdrawal effects. Such patients do not abuse other drugs and only a minority over-indulge in alcohol.
High dose benzodiazepine dependence is often combined with abuse of other drugs. Most polydrug abusers throughout the world today also abuse benzodiazepines. These individuals take benzodiazepines irregularly, often in doses ten times or more greater than 'therapeutic' users and may inject intravenously - particularly temazepam in the UK. The capsule form of this drug (commonly used for intravenous injection) was withdrawn in the UK in 1996, but tablets are still available. The drugs are used recreationally to obtain a 'high', to increase the 'high' obtained from other recreational drugs, and/or to alleviate the abstinence syndrome from other drugs of abuse (opiates, cocaine, amphetamine). For some of these individuals, benzodiazepines were initially prescribed by doctors.
Although the two types of benzodiazepine dependence generally involve different populations, there is (iii) an intermediate group in which individuals may have started on prescribed benzodiazepines but have escalated their dosage, take more than their prescribed doses and drift from doctor to doctor or visit hospital casualty departments in order to obtain increased supplies which they self prescribe. Sometimes, though not always, this group combines benzodiazepine misuse with excessive consumption of alcohol.
The different populations of benzodiazepine-dependent persons manifest various degrees of 'addictive', features. All exhibit drug-seeking behaviour: prescribed dose users by regular visits to their doctors to obtain repeat prescriptions; high dose abusers by prescription forgeries, theft or purchase from illegal suppliers. All manifest psychological dependence on their drugs in that they become anxious if a ready supply is not available. Therapeutic dose users often carry their tablets around with them and not uncommonly take an extra dose before an anticipated stressful event or, in the case of hypnotic users, a night in a strange bed. They make sure to obtain the next prescription before the previous supply has run out. Higher dose users concoct ingenious stories in order to obtain prescriptions: some personally experienced examples include 'taken by teenage daughter'; 'put in garbage bin by mistake just before bin collected'; 'stolen with purchases in shopping centre'; 'left in flat from which subject ejected', etc.
Such behaviour is evidence of a strong desire or perceived 'need' for the drugs in all types of dependent users.
EXPERIMENTAL STUDIES OF DEPENDENCE POTENTIAL: REINFORCEMENT
The reinforcement potential of a drug is judged by its ability to maintain or increase the frequency of drug-taking or drug-seeking behaviour. Positive reinforcement is assumed to be associated with some 'rewarding' or hedonic effect directly exerted by the drug, while negative reinforcement is associated with a drug's ability to alleviate aversive or 'punishing' states such as anxiety or withdrawal symptoms.
Positive reinforcement by benzodiazepines has been hard to demonstrate in animals or man. In animals, strongly reinforcing drugs such as amphetamines or cocaine are readily and repeatedly self administered after suitable priming and are preferred to placebo. Such self administration of benzodiazepines has not been consistently demonstrated in animals. Indeed, in an extensive review of the literature Woods, Katz & Winger (1992) state that 'across a wide range of conditions, benzodiazepines generally do not maintain appreciable self administration behaviour' (p.168). In certain experimental situations benzodiazepines can maintain self-administration, but much less potently than barbiturates and other drugs of dependence. On the other hand, there is much evidence that benzodiazepines provide negative reinforcement. They reverse the behavioural inhibition produced by electric shocks paired with food reward, the Geller-Seifter procedure, and that produced by several anxiogenic procedures in rodents (File & Baldwin, 1989). Whether or not self-administration is increased in aversive situations, especially in withdrawal states in benzodiazepine-dependent animals is at present not clear.
The avidity with which animals will self administer drugs shows some parallels with drug preference and 'liking' scores in human subjects (Warburton, 1988). In drug preference tests the subject, after previous experience of taking a range of drugs and placebo in colour-coded capsules, chooses which capsule to take over several occasions in constant experimental conditions. The tests are usually combined with subjective ratings of mood and of hedonic or euphoriant effects ('liking' scores). In line with animal studies, normal subjects and anxious volunteers show no preference or increased liking compared with placebo for a variety of benzodiazepines in several doses within the therapeutic range. In contrast, amphetamine (5 mg) is significantly preferred by normal subjects, though not by anxious volunteers. Among abusers of other recreational drugs 'liking' scores for benzodiazepines are low compared to other drugs (Fig. 2) and scores for drugs of abuse in general correlate with their potency as positive reinforcers in animals.

Nevertheless, reinforcing effects of benzodiazepines are apparent in particular human populations: (i) in patients with psychoneurotic disorders to whom benzodiazepines are available on demand, the amount of drug requested is related to the degree of anxiety, and anxious subjects seeking treatment prefer benzodiazepines to placebo; (ii) patients undergoing abrupt benzodiazepine withdrawal show a preference for benzodiazepines and self-administer them when available; (iii) insomniac subjects express significantly increased liking for benzodiazepines over placebo when offered as an aid to sleep; (iv) subjects with a history of sedative drug abuse show preference and increased 'liking' scores for benzodiazepines, especially in high doses; (v) benzodiazepines also have greater reinforcing effects in subjects with a history of alcohol abuse compared to non-alcohol abusers and in normal subjects with a history of moderate alcohol consumption compared to those with low levels of alcohol consumption.
Thus both human and animal studies show that benzodiazepines in therapeutic doses have little potency as positive reinforcers; they do, however, act as negative reinforcers, alleviating anxiety and withdrawal states. As argued elsewhere (Ashton, 1989) benzodiazepines act essentially as 'depunishing' rather than as directly rewarding drugs. High doses (in the range of 100 mg diazepam or more) may have positive reinforcing effects in some subjects, notably abusers of other sedative drugs, a finding in agreement with the testimony of intravenous temazepam users. These individuals and those with a history of excessive alcohol use are at particular risk of developing high dose benzodiazepine dependence, while anxious patients with certain dependent personality traits are at risk of low dose dependence (Tyrer, 1987; Ashton, 1989).
TOLERANCE
Dependence on many drugs of addiction is linked with the development of tolerance, an adaptive state which develops on repeated administration such that larger doses are required to elicit the original effect. Tolerance to the actions of benzodiazepines, including anxiolytic effects, has been demonstrated in animals (File & Baldwin., 1989). In man, a remarkable degree of tolerance can develop in high dose benzodiazepine users. For example, a patient taking 240 mg diazepam and 240 mg oxazepam daily (confirmed by blood concentrations) regularly rode a bicycle and also passed a written English examination with merit. The patient was still highly anxious, suggesting tolerance to the anxiolytic as well as to the hypnotic and ataxic effects of the benzodiazepines. Patients on therapeutic doses rapidly develop tolerance to hypnotic effects of benzodiazepines; tolerance to anxiolytic effects seems to develop more slowly but may lead to dosage escalation or 'break-through' anxiety on fixed doses.
The mechanisms of benzodiazepine tolerance are not fully understood but may involve down-regulation of affinity or density of gamma-aminobutyric acid (GABA)/benzodiazepine receptors in the brain (Nutt, 1986), or possible alterations in activity of putative endogenous benzodiazepine-like substances (File & Baldwin, 1989). There is little doubt that chronic use of benzodiazepines causes profound adaptive changes in the brain. Such changes may be largely responsible for withdrawal effects on drug cessation, and clinical experience suggests that long-term users take benzodiazepines more to prevent withdrawal effects than to alleviate the condition for which they were originally prescribed.
PHARMACOLOGICICAL DEPENDENCE: WITHDRAWAL EFFECTS
Pharmacological (or physiological) dependence is defined as a state which develops during chronic drug treatment in which cessation of the drug (or administration of a pharmacological antagonist) elicits an abstinence reaction which is time limited and is reversible by renewed administration of the drug. Animal studies have consistently shown that all benzodiazepines are capable of inducing physiological dependence after chronic administration. Withdrawal signs differ between species and the intensity and duration of the withdrawal syndrome depends on drug dosage, duration of administration, and to some extent on type of benzodiazepine. It is not clear to what degree withdrawal effects are influenced by the extent of previous drug tolerance.
It has been known for some time that high doses of benzodiazepines produce pharmacological dependence in man and that abrupt cessation after chronic use can cause severe withdrawal phenomena such as convulsions and psychotic reactions. The existence of dependence in long-term therapeutic dose users was established by placebo-controlled clinical studies (Petursson & Lader, 1981; Owen & Tyrer, 1983) and the human benzodiazepine withdrawal syndrome was described. This syndrome, which is similar to the abstinence syndrome of other sedative/hypnotic drugs and of alcohol, consists of a large constellation of somatic and psychological symptoms. The clinical picture is mainly that of anxiety, but certain symptoms such as sensory hypersensitivity and perceptual distortion appear to be especially prominent. The non-specific nature of the symptoms and the fact that anxiety is often present before withdrawal makes definition of the syndrome difficult (Ashton, 1991). 'Pseudowithdrawal' anxiety may occur in patients who believe their benzodiazepines are being withdrawn and a distinction is traditionally made between psychological and pharmacological dependence. However, anxiety in the face of anticipated drug deprivation is itself a feature of dependence (and involves physiological changes in CNS activity), and treatment is the same whether the symptoms are true or 'pseudowithdrawal' symptoms.
The incidence of the withdrawal syndrome is not clear. Estimates vary, depending on factors such as definition and measures of withdrawal symptoms, selection of patients, and rate of withdrawal. Such estimates do not usually take account of dropouts (often due to severe withdrawal symptoms) or of those who decline to undergo withdrawal (50-100% of eligible patients in some studies). In general a withdrawal syndrome is believed to occur in 30-45% of patients who have used regular therapeutic doses of benzodiazepines for more than a few months, but the incidence varies between less than 20% and 100% in different studies. It is not clear why some chronic users apparently do not become dependent; and if not dependent why they continue drug use over many years. However, drug dependence is not an absolute; it can exist in many different degrees.
The duration of the withdrawal syndrome is also debatable. Classically symptoms subside to prewithdrawal levels within 4-6 weeks, but some symptoms may decline more slowly, merging into a period of increased vulnerability to stress which may be partly a consequence of learned behaviour related to drug taking (Ashton, 1991; Owen & Tyrer, 1983). Certain potent, rapidly metabolised benzodiazepines (alprazolam, triazolam, lorazepam) have been associated with more severe withdrawal symptoms, possibly because of their greater potency. Because of their short half lives, the onset of withdrawal is also more acute and withdrawal symptoms may occur between doses (inter-dose anxiety). Dosage (within the therapeutic range) and duration of benzodiazepine use (above 6-12 months) do not appear to affect the incidence or severity of withdrawal, but anxious and passive-dependent personality types (Owen & Tyrer, 1983) and alcohol-dependent subjects may be especially vulnerable. High dose benzodiazepine abusers are at almost certain risk of withdrawal symptoms unless dosage tapering is extremely slow.
BENZODIAZEPINE CONSUMPTION
Consumption of benzodiazepines is still enormous worldwide (for a review of the epidemiology, see Woods et al., 1992). Although prevalence of benzodiazepine use has recently declined in many countries, 10.9% of the US population surveyed in 1990 reported having used benzodiazepines during the previous year. In the UK prevalence, as thus defined, fell from 11.2% in 1981 to about 3.3% in 1986 (lower than in most European countries). These decreases resulted mainly from changes in tranquilliser use; hypnotic use has remained relatively stable since 1981 (Table 1 shows benzodiazepines marketed as tranquillisers and hypnotics).
Note: The pharmacological actions of all benzodiazepines
are similar; the distinction between tranquillisers and
hypnotic preparations is based on commercial,
not pharmacological,
grounds.
*Withdrawn UK in 1991
Meanwhile sales of benzodiazepines have risen markedly in the US and most European countries, except the UK where sales have fallen. The discrepancy between general trends in prevalence of use and sales of benzodiazepines suggests the existence of a growing cohort of long-term regular benzodiazepine users, as presaged by Owen and Tyrer in 1983. Population surveys support this interpretation, and about 2% of the adult populations of the US (ca. 4 million people) and of the UK (ca. 1 million people) appear to have used benzodiazepine hypnotics or tranquillisers regularly for 12 months or over; 50% of these for 5-10 years or more. A high proportion of these users must be assumed to be at least to some degree dependent on benzodiazepines.
Amongst the chronic benzodiazepine users, females outnumber males by 2 : 1 and use is related to age. Frequency of use of anxiolytic benzodiazepines increases up to 50-65 years of age, while hypnotic use continues to rise to a peak at 65 years or over. Such use may be related to the higher prevalence of anxiety disorders in younger age groups and of insomnia amongst the elderly, but it should be noted that the pharmacological actions, dependence potential and incidence and type of withdrawal symptoms is similar for all benzodiazepines, whether marketed as hypnotics or as anxiolytics. Prevalence of physical and psychological ill-health and scores for trait and state anxiety are significantly higher amongst chronic benzodiazepine users than in the general population. The extent to which benzodiazepines are prescribed and used for sociological reasons and as psychological coping strategies is discussed by Gabe (1991).
Prevalence of benzodiazepine use as primary recreational drugs is claimed to be trivial compared with other drugs of abuse (Woods et al., 1992), but reports from many countries show that a large proportion (30-90%) of polydrug; abusers, especially opiate abusers, also abuse benzodiazepines. Benzodiazepines used orally for recreational purposes include diazepam, alprazolam, temazepam, flunitrazepam and, to a lesser extent, triazolam and lorazepam. Temazepam is also injected intravenously and its use in combination with the opiates buprenorphine and dihydrocodeine appears to be particularly common amongst intravenous drug abusers in Scotland. The population of recreational benzodiazepine users is perhaps a tenth of that of chronic prescribed users, but probably amounts to some hundreds of thousands in the US and UK, and may be increasing.
ADVERSE EFFECTS OF LONG-TERM BENZODIAZEPINE USE
Growing experience with benzodiazepines in the 1980s led many patients and professionals to question the value of long-term use. Disadvantages of chronic benzodiazepine use include psychomotor, cognitive and memory impairment, interactions with other sedative drugs such as alcohol, emotional clouding, depression, and sometimes paradoxical excitement and aggressiveness. Sociological costs may include increased risk of traffic and other accidents, falls and fractures in the elderly, shoplifting (due to amnesia) and violent behaviour (due to paradoxical effects). Furthermore, dependence and withdrawal reactions make it difficult for many long term users to stop taking benzodiazepines despite adverse effects.
RATIONAL USE OF BENZODIAZEPINES
Although benzodiazepines are highly effective in short-term treatment for anxiety and insomnia, in long-term use the risks of dependence and other adverse effects outweigh the benefits (Tyrer, 1987). Most authorities in the UK, recommend that the use of benzodiazepines should be limited where possible to short-term (maximum 4 weeks) or intermittent courses, in minimal effective doses, prescribed only when symptoms are severe (Committee on Safety of Medicines, 1988; Royal College of Psychiatrists, 1988; Consensus Conference, 1992; Drug and Therapeutics Bulletin, 1990). It is recognized that psychological treatments (sometimes combined with antidepressants) are more appropriate in the longer term for most patients with anxiety disorders.
The management of patients already dependent on benzodiazepines is described in detail elsewhere (Ashton, 1994). Essentially it consists of gradual, individualised and patient-controlled dosage reduction (usually over a period of months) combined with individual psychological support. Adjuvant drugs such as beta-blockers, carbamazepine, buspirone and others have not been found to be generally helpful, but antidepressants may be indicated if depression is severe. Animal studies (and limited clinical experience) suggest a potential use for drugs which act as partial agonists or antagonists at benzodiazepine receptors. The outcome of withdrawal for therapeutic dose users who are motivated to withdraw is good: abstinence rates 1-5 years after withdrawal vary between 54% and 92% in different studies, and there is no evidence of increased alcohol use or psychiatric morbidity in those who withdraw successfully. For patients unwilling to withdraw continued prescribing in minimal doses may be necessary. Long-term follow-up information on high dose abusers is scarce but withdrawal failures and relapse rates appear to be higher than in therapeutic dose users.
THE FUTURE
With rational prescribing, benzodiazepines are likely to remain useful drugs for short-term use. Prevalence of use should continue to decline as the number of chronic users decreases and fewer new patients become dependent. The medical profession should be cautious in prescribing new non-benzodiazepine anxiolytics and hypnotics now appearing on the market. Such successors to benzodiazepines, if used as chronic treatments, may not be without a dependence potential similar to that of benzodiazepines.
REFERENCES
Ashton, H. (1989). Risks of dependence on benzodiazepine drugs: a major problem of long-term treatment. British Medical Journal, 298, 103-4.
Ashton, H. (1991). Protracted withdrawal syndromes from benzodiazepines. Journal of Substance Abuse Treatment, 8, 9-28.
Ashton, H. (1994). The treatment of benzodiazepine dependence. Addiction, 89, 1535-41.
Committee on Safety of Medicines. (1988). Benzodiazepines, dependence and withdrawal symptoms. Current Problems, 21.
Consensus Conference. (1992). Guidelines for the management of patients with generalised anxiety. Psychiatric Bulletin, 16, 560-5.
Drug and Therapeutics Bulletin. (1990). The treatment of insomnia. Drug and Therapeutics Bulletin, 28, 97-9.
File, S.E. & Baldwin, H.A. (1989). Changes in anxiety in rats tolerant to, and withdrawn from, benzodiazepines: behavioural and biochemical studies. In P. Tyrer, (Ed.), The psychopharmacology of anxiety, pp. 28-51, Oxford: Oxford University Press.
Gabe, J. (1991). Personal troubles and public issues: the sociology of long-term tranquilliser use. In J. Gabe (Ed.)., Understanding tranquilliser use: the role of the social sciences, pp. 31-47, London: Tavistock/Routledge.
Nutt, D. (1986). Benzodiazepine dependence in the clinic: reason for anxiety? Trends in Pharmacological Sciences, 7, 457-60.
Owen, R.T. & Tyrer, P. (1983). Benzodiazepine dependence: a review of the evidence. Drugs, 25, 385-98.
Petursson, H. & Lader, M.H. (1981). Benzodiazepine dependence. British Journal of Addiction, 76, 133-45.
Royal College of Psychiatrists. (1988). Benzodiazepines and dependence: a College statement. Bulletin of the Royal College of Psychiatrists, 12, 107-8.
Tyrer, P. (1987). Benefits and risks of benzodiazepines. In H. Freeman & Y. Rue (Eds.). The benzodiazepines in current clinical practice, pp. 3-11, London: Royal Society of Medicine Services.
Warburton, D.M. (1988). The puzzle of nicotine use. In M. Lader (Ed.). The psychopharmacology of addiction, pp. 27-49, Oxford: Oxford University Press.
Woods, J.H., Katz, J.L. & Winger, G. (1992). Benzodiazepines: use, abuse and consequences. Pharmacological Reviews, 44, 151-338.
